
Enabling Health Plans To Meet CalAIM Requirements
What is CalAIM
CalAIM is California’s groundbreaking effort to improve the lives of the Medi-Cal population by meeting people where they are, addressing social drivers of health, and breaking down barriers in accessing care. This population health approach prioritizes prevention and whole-person care.
An Opportunity for Joint Innovation
To navigate this dynamic environment and deliver comprehensive care to vulnerable populations, health plans need innovative solutions that go beyond traditional healthcare delivery services. That’s where Unite Us comes in.
CalAIM recognizes the need for a broader delivery system, program, and payment reform across the Medi-Cal program, making collaboration and coordination across sectors essential to address complex challenges such as homelessness, behavioral health care access, and the needs of justice-involved populations. Since Unite Us’ launch in 2013, we have established an industry standard for social care coordination. With best practices ensuring that people receive the care they need and accountable networks in every county, we are on the ground in California to meet the needs of health plans and the communities they serve to meet the state’s ambitious goals for population health.
For health plans and community organizations alike, ease of use is top of mind. We connect clinical and community organizations, delivering an intuitive coordination experience and reducing the risk of errors and inefficiencies, thanks to integrated workflows and tools: from screenings and eligibility to referrals and follow-ups. Our secure infrastructure for information exchange allows for a single member record and an integrated view across medical and non-medical services so as to enable non-duplicative, member-centered care across multiple touchpoints. A Unite Us partner at Florida health system identified 3.97 hours saved per case manager per week, resulting in an annual cost savings of $7,225 per case manager in a research and evaluation study.
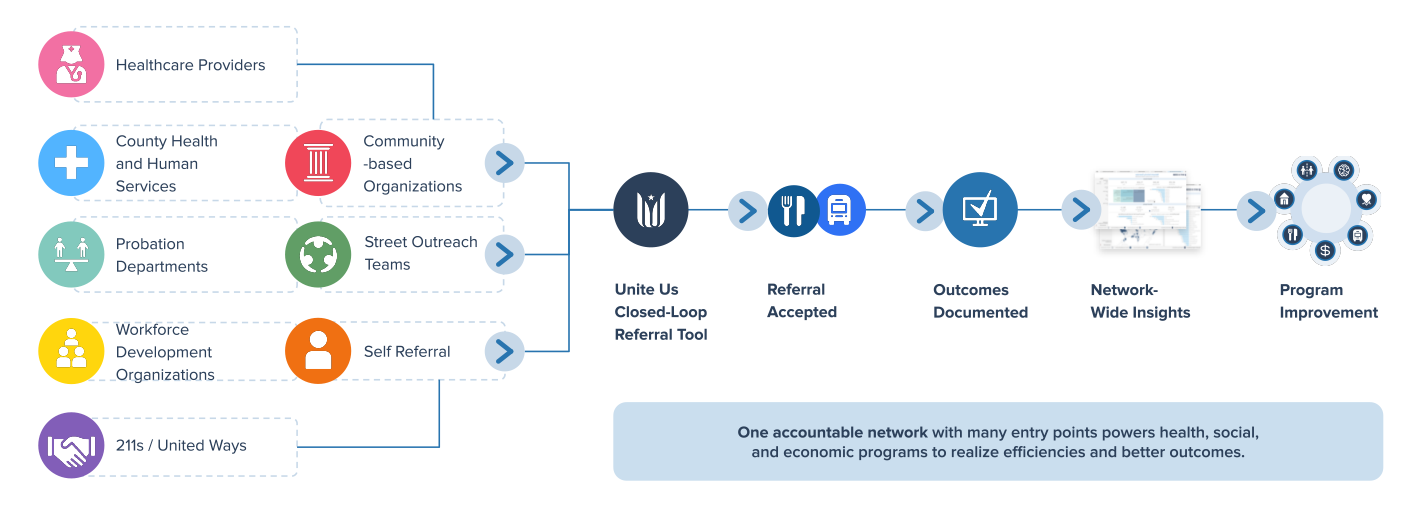
Unite Us is the only vendor that has built a responsive and accountable social care network across California that provides real-time connectivity—supporting the upcoming DHCS requirement for a closed-loop referral system. We’ve partnered with population health management organizations, such as county agencies and community-based organizations, to help health plans swiftly contract and onboard community partners ready to serve your members. Our continuous training and user engagement ensure adoption and appropriate utilization. We support partners in achieving their goals and monitor network activities to understand how population needs evolve.
Identifying Social Needs and Connecting People to Services
Unite Us provides a powerful interoperable platform that makes it easy to screen for social needs, identify the most suitable resources, and securely connect individuals to the services that can make a difference in their lives. In a fragmented healthcare landscape where individuals may need access to multiple delivery systems, Unite Us streamlines the process, ensuring that people receive holistic care.
CalAIM seeks to identify and manage member risk and needs through whole-person care approaches and addressing social determinants of health. Within CalAIM, Enhanced Care Management (ECM) and Community Supports (CS) are foundational parts of the transformation focused on:
- Breaking down the traditional walls of health care, extending beyond hospitals and health care settings into communities;
- Introducing a better way to coordinate care; and
- Providing high-need members with in-person care management where they live.
This aligns with Unite Us’ mission to connect communities and improve well-being by addressing social needs and disparities. By leveraging the Unite Us Platform and network, ECM and CS partners across California are securely making closed-loop referrals without manual or duplicative efforts.
Data-Driven Impact Measurement
Building healthier communities requires more than just addressing immediate challenges. It demands a data-driven approach to understand what works, what doesn’t, and how to scale impact across providers and networks. Unite Us offers our Platform and Insights Center as tools for health plans to comprehensively understand the members’ needs and outcomes of care delivery.
CalAIM aims to track, in real-time, the impact of reducing disparities and improving health outcomes. With Unite Us, health plans can achieve this goal by measuring the effectiveness of their social care strategy and developing a data-driven population health management strategy. Unite Us’ data offerings include:
- The ability to standardize social care information, with over 700 referral and service outcomes to understand gaps and opportunities and ensure investments are working
- Secure information exchange infrastructure that is HIPAA-compliant and HITRUST, NIST, and SOC-2 certified
- Data-driven insights to proactively identify social care needs, as well as communication preferences to support enrollment into Enhanced Care Management and Community Supports Services
To avoid duplicative data entry and managing multiple data systems across settings, Unite Us offers a centralized, seamless experience that prioritizes the patient’s privacy first. When a Medi-Cal member gives consent to a provider to connect them to services through Unite Us, we ensure that their information will be protected and secure. That’s why we protect social care information under the same strict security standards required for protected health information under HIPAA and apply heightened protections for sensitive information such as 42 CFR Part 2-covered information.
Reimbursement for Social Care
Healthcare providers are reimbursed for the services they provide, and Unite Us believes that the same principle should apply to social care. With Unite Us Payments, funders can reimburse community-based organizations at scale, which can include Community Support and Enhanced Care Management Providers, for the services they already provide while measuring the success of social care funding initiatives over time.
Unite Us Payments simplifies the grant tracking, billing, enrollment, and authorization processes, aligning with CalAIM’s commitment to simplifying and scaling social care funding. This will centralize complex coding and rate information, boost efficiency, and scale impact while reducing risks of costly denials and rejections.
As an Enhanced Care Management and Community Support provider, we use Unite Us mainly for billing and so far, we have found the platform to be very user-friendly. We have also enjoyed the support from the Unite Us staff when dealing with minor issues and questions. The Unite Us Platform not only allows us to invoice for our clients but also to interact with other community support and thus extend the services we are able to provide for our clients. – Merced County Rescue Mission
Enhancing Health Plan Outcomes
Hidden social needs can significantly impact the outcomes and experiences of health plan members. Aligning with CalAIM’s goal to improve quality outcomes and drive delivery system transformation, health plans can use Unite Us to:
- Better identify health-related social needs and risks in their population.
- Coordinate with responsive community partners for targeted interventions.
- Simplify reporting and demonstrate how they addressed diverse needs.
In the era of CalAIM, collaboration and innovation are key to achieving better health outcomes for California’s most vulnerable residents. Partnering with Unite Us empowers health plans to connect communities, streamline social care, measure impact, and simplify funding – ultimately improving the lives of the members they serve.
This is an opportunity to innovate, adapt, and grow with us!
About Unite Us
Unite Us is the nation’s leading software company bringing sectors together to improve the health and well-being of communities. We drive the collaboration to identify, deliver, and pay for services that impact whole-person health. Through Unite Us’ national network and software, community-based organizations, government agencies, and healthcare organizations are all connected to better collaborate to meet the needs of the individuals in their communities.



